- Received June 07, 2024
- Accepted August 12, 2024
- Publication October 10, 2024
- Visibility 3 Views
- Downloads 0 Downloads
- DOI 10.18231/j.ijohd.2024.031
-
CrossMark
- Citation
Evaluation of maxillary sinus in health and disease through CBCT imaging: A literature review
- Author Details:
-
Priyanka Khanna *
-
Priya Singh
-
Deepak Umapathy
-
Shweta Singh
Introduction
The biggest paranasal sinus in the cranium is the maxillary sinus (MS), which begins on the side of the nose and extends all the way to the zygomatic process of the maxillary bone. The shape is pyramidal. The canalis sinuosus, which also contains the anterior superior alveolar nerve and blood vessels and the maxillary facial bone form and groove the interior of the MS's anterior wall. The slender canine fossa, the infraorbital foramen in the mid superior area and the infraorbital groove are three prominent markers on the anterior wall.[1], [2], [3], [4], [5]
A person's maxilla's infratemporal surface forms the posterior wall. Along its front edge, it creates the pterygopalatine fossa. The infraorbital groove cuts through the delicate triangular orbit floor, which forms the superior wall. On average, the sinus roof is 0.4mm thick medial to the infraorbital canal and 0.5 mm thick laterally to it and it becomes thicker as it approaches the orbital edge.[6], [7], [8], [9]
The MS's medial wall divides the nasal cavity and sinus. It supports the inferior nasal conchae on the nasal side and is smooth on the sinus side. At the maxillary hiatus, there is a little deficiency in the medial wall, which is rectangular in form.[10], [11] In an enunciated skull, the ostium and front and rear fontanelles are formed by the sub-par turbinate, the uncinate cycle of the ethmoid bone, the lacrimal bone, the opposite plate of the palatine bone and the covering mucosa, which partially close this aperture. After passing through the semilunar fissure and into the central nasal meatus, the ostium opens onto the inferior portion of the ethmoidal infundibulum.
Possible anatomic variations include, alveolar pneumatisation antral septa, aberrant mucosal thickness, hypoplasia and exostosis, maxillary sinus hypoplasia (MSH). The maxillary sinus hypoplasia (MSH) may occur either during embryological development or as a result of injury, iatrogenic factors, or other underlying conditions. Because the hypoplastic sinus lacks a distinctive ostium, it experiences mucosal thickening due to restricted infundibular entrance. On top of that, MSH makes procedures more difficult by causing the horizontal nasal wall to enlarge at its proximal end. The septa of the maxillary sinus act as barriers to the cortical bone. The maxillary sinus floor is divided into many compartments, called breaks, by the second rate or parallel sinus walls, from which the shape emerges as a converted gothic curve. Anatomist Arthur S. Underwood was the first to study these septa and describe their characteristics; as a result, they are often referred to as Underwood's septa.[7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18]
Among the imaging modalities that may be utilized to examine the area surrounding the maxillary sinuses are Panorama, Waters, Caldwell, Computed Tomography (CT), Magnetic Resonance Imaging (MRI) and Cone Beam Computed Tomography (CBCT). For a long time, cranial projections such as Waters, Caldwell and lateral sinus were used for paranasal sinus examinations. In order to get a good look at the maxillary sinus, it's useful to use the water's view.[18], [19], [20] This is particularly true if you are looking for evidence of radiopacification, locally distributed mucosal lining thickening along the sinus floor, or mucosal lining thickening across the sinus wall.[21], [22], [23], [24], [25], [26], [27]
Nowadays, plain films are seen as supplementary to more advanced imaging techniques. Because they can only show structures in two dimensions they can only provide a high-level picture of the anatomy and underlying pathoses. One benefit of CT and MRI over plain films is that it may display precise anatomic features in serial topographic slices, without the bulk volume averaging that is present in plain films. CT or MRI is the next step after a plain-film investigation confirms the disease's appearance. With CBCT a single rotation may collect several projections using a cone or pyramidal-shaped beam.[28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41]
Potential problems that may arise after sinus floor elevation surgery are strongly influenced by the unique anatomy of the maxillary sinus. Prior research has shown a wide range of anatomical trait prevalence. In addition, other studies found different correlations between different anatomical features and age, oral health and sex. CBCT has a little higher radiation exposure than regular panoramic radiography for dento-maxillofacial imaging, although it may be suggested as a cost-effective method of dose reduction when compared to conventional medical Multi-detector computed tomography scans (MDCT).[41], [42], [43], [44], [45], [46] “The international commission on radiological protection found that compared to similar medium-field of view dental CBCT scans, the effective dosage from a conventional dental protocol scan using multidetector computed tomography (MDCT) is 1.5 to 12.3 times higher (ICRP 2007).” Dental materials (such as amalgam, crowns and implants) and beam hardening artifacts are less pronounced during CBCT compared to Multi-slice spiral computed tomography (MSCT). Being well-versed on the various anatomic and pathologic findings in the sinuses is essential for minimizing the risk of postoperative problems after maxillary sinus floor lifts and other procedures in this area.[47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62] The maxillary sinuses are essential anatomical structures in dentistry, thus it's crucial to have a precise radiological evaluation of them. CBCT is a valuable diagnostic imaging modality for this purpose.
Lana JP et al.[35] performed research to assess the accuracy of cone beam computed tomography (CBCT) scans of the maxilla, which are necessary for dental implant design, in identifying anatomical variables and pathologies of the maxillary sinus. It was found that CBCT scans of the maxilla, which are necessary for dental implant design, often revealed anatomical abnormalities and maxillary sinus infections. Particularly in the field of implantology, the identification of these diseases is significant since they might alter dental implant planning and need specialist treatment. This study's findings on anatomical differences and lesions, both in number and significance, highlight the use of computed tomography for dental implant preoperative planning.
“Hence, the purpose of the current article was to determine the anatomical and morphological variations which are important to know to adjust the treatment plan to yield more successful results using CBCT.
Methodology
A literature review was performed using the PubMed, MEDLINE and Scopus databases, Google scholar from year 1986 to 2024 for the normal anatomy and development of maxillary sinus and their pathologies. A review of pertinent literature on the anatomy and diseases of the maxillary sinus on CBCT imaging was conducted, with a focus on its morphology.
Discussion
Anatomy
Posterior superior alveolar artery (PSAA) and lateral wall thickness
The lateral part of the maxillary antrum and the Schneiderian layer overlying the lateral portion of maxillary antrum are supplied by the PSAA, an extension of the maxillary artery. Deep bleeding is a possibility that should be thoroughly assessed during sinus grafting surgeries. There have been reports of excessive bleeding following PSAA damage during augmentation of base of maxillary antrum using the transcrestal approach. On CBCT scans, probability of visualization and detection of PSAA varied from approximately 49% to 92%. PSAA was less common at the outermost region of the antrum lateral wall (5 to 10%), while it was more common beneath the membrane that covers the sinus (13 to 16%) or found intraosseously (29% to 72%).[12], [13], [14], [15], [16], [17], [18] Because PSAA is minuscule and lies closely on both ends of the maxillary antrum lateral wall without creating a bone depression, it may appear to be absent in CBCT images.[63], [64], [65], [66], [67], [68], [69], [70], [71], [72], [73], [74]
In the meantime, CBCT imaging may be used during interventions for augmentation of floor of maxillary sinus to assess the maxillary sinus's lateral wall thickness. The overall average thickness of lateral wall of maxillary antrum was determined to be 1.6 ± 0.8 mm measured at both four millimeters apically and six millimeters apically or superiorly to floor of maxillary antrum in a retrospective examination of 209 individuals presenting with CBCT images.[19], [20], [21], [22], [23], [24], [25], [26], [27]
On the other hand, the average lateral wall thickening of the instances with perforation of antrum membrane during the surgery was 2.4 ± 0.6 millimeters at both four millimeters and six millimeters apically to the floor of maxillary antrum, while the non-perforation patients had an average thickness of 1.2 ± 0.4 millimeters. Additionally, it was discovered that the thickness of maxillary antrum lateral wall is significantly linked with leftover ridge height and significantly thicker in individuals with partial edentulism than in circumstances of full edentulism. The thickness of the maxillary antrum lateral wall and the measurement of the diameter of PSAA exhibited a favorable connection.[28], [29], [30], [31], [32]
The frequency of inadvertent maxillary sinus discoveries in orthodontic cone-beam computed tomography (CBCT) pictures was examined by Pazera P et al. in their 33-" study. Of all CBCTs, 65 had incidental abnormalities in the maxillary sinus, accounting for 46.8% of the total. Three types of accidental observations were found: flat mucosal thickening (23.7%), polypoid mucosal thickening (19.4%) and acute sinusitis symptoms (3.6%). Incidental maxillary sinus abnormalities unrelated to the main reason are seen in a significant number of CBCTs performed for orthodontic diagnostic purposes.
Pneumatization
The constant expansion of the paranasal sinuses, a condition known as sinus pneumatization, is a normal physiological function. A person's sinuses make their voice more resonant, help shape their face and even warm and humidify the air that is inspired to a certain extent. Localized alterations in the dimensions of both hard and soft tissues are facilitated by tooth loss. Implant placement at the back of the upper jaw might be challenging due to the presence of maxillary sinus approximation and bone loss. The maxillary sinuses, out of the four paranasal sinuses, are the most relevant to dental care because of their close proximity to teeth. The process of pneumatization occurs when the sinuses cavities are created and filled with air during the development of the maxillary bone.[34], [35], [75], [36], [37], [38], [39], [40], [41], [42] The most common anatomical area is the alveolar process, however pneumatization also causes the maxillary sinuses to enlarge into neighboring tissues. A lot of people still don't understand the procedure. Genetics, craniofacial traits, bone density, sinus operations, growth hormones, air pressure inside the sinus cavity, natural aging and nasal mucous membrane pneumatization are some of the factors that have been shown to influence maxillary sinus pneumatization in clinical studies.[43], [44], [45], [46], [47], [48]
In a population from southern Iran, Shahidi S et al.,(2016)[49] employed CBCT to determine normal variations of the maxillary sinus. Axillary images were employed to evaluate a range of anatomic anomalies, including anterior pneumatization, exostosis and hypoplasia. The precise positioning of the PSAA and the height and location of the sinus septa were also assessed. The study discovered that there were frequent anatomical variations in the maxillary sinuses in maxilla CBCT. Preoperative CBCT imaging appears to be quite helpful in better analysing the maxillary sinus architecture and PSAA placement prior to surgery. The surgical treatment plan may then be adjusted using this information to get improved results.
A narrative review of the application of cone beam computed tomography (CBCT) in evaluating the architecture and common disorders of the maxillary sinuses was presented by Yeung AWK et al.,(2022).[68] Information was given on the location, morphometric properties and rate of detection and visualization. Anatomical features of the sinuses that were investigated included pneumatization of the sinuses, hypoplasia, septa, main and auxiliary sinus ostia and the posterior superior alveolar artery. The pathology assessment included antrolith, mucous retention cysts and membrane thickening in periapical/ periodontal lesions. Procedures that include the extraction of teeth, the insertion of implants or the elevation of the sinus floor are all performed in close proximity to the sinus floor, thus it is crucial to observe and evaluate the maxillary sinus before these operations. Periodontal bone loss and other sinus pathologies might be accompanied with odontogenic lesions.
|
Authors |
Origin |
Objective |
Age group /status |
Findings |
Conclusion |
|
Al-Zahrani MS et al (2020)[63] |
Saudi population |
Using cone beam computed tomography (CBCT) to find out how often septa are seen, how they look like and how they relate to age and gender |
Adult /Healthy |
There were 370 sinuses (or 37% of the total) with maxillary septa, affecting around 46% of the participants in the study. Approximately 64% of the septa were located on the right side and 85% of the septa were orientated medially. For the right sinuses, the average septal height was 6.06mm (0.84), whereas for the left sinuses, it was 5.70mm (0.93). One hundred ten individuals, or 20% of the total, had multiple septa. In contrast to 34% of females, 58.5% of men exhibited septa |
The presence and quantity of septa were positively correlated with age. The majority of the subjects in the study had maxillary sinus septa, which might be any height or orientation. Prior to maxillary sinus augmentation, it is crucial to thoroughly evaluate various anatomic variations, especially in elderly individuals. |
|
Pei J et al (2020)[64] |
Western Chinese population |
Exploring the connection between the maxillary sinus and the first and second molars using cone-beam computed tomography in a sample of western Chinese people |
Adult/ Healthy |
In terms of the space between the maxillary sinus and the roots of the upper teeth, neither sex nor side had any bearing. The maxillary sinus, which is located between the roots of the upper teeth, becomes broader as individuals age. The second tooth's mesiobuccal root was closest to the maxillary sinus. |
When there was a cross-section of the maxillary sinus above the root apex and the root was not contacting the sinus border, the majority of associations occurred. The back teeth of the upper jaw are unlike any other teeth because of their intricate architecture and their close relationship to the sinus. For patients in western China undergoing dental clinical treatments such as root canal therapy, tooth extraction, dental implant, etc., these results may provide useful reference information. |
|
Toprak ME et al (2021)[65] |
Turkish population |
Using cone beam computed tomography (CBCT) to examine the frequency, shape, location, origin, orientation of maxillary sinus septa in dentate, fully edentulous and partly edentulous sinus areas and potential patient-related variables were also considered. |
Adult/ Healthy |
Results showed that middle third area of totally edentulous sinus areas had a much greater incidence of septa. In 204 patients (98.08%), the average septal height was 6.34 (3.05)mm and the average orientation was bucco palatal. |
Anatomical structures that are often seen include maxillary sinus septa. An accurate radiographic characterization of the anatomical components in the maxillary sinuses is necessary to prevent any difficulties during sinus augmentation. |
|
Shaul Hameed K et al (2021)[66] |
Saudi population |
Using Cone beam computed tomography (CBCT) was used to assess the horizontal and vertical connection types of posterior root apices to the maxillary sinus floor (MSF) in the Al-Qassim (Saudi) population |
Adult/ Healthy |
The average distance between the apices of the second premolars in the upper jaw was between 4.63 and 6.49mm. On the right second molar of the maxilla, the average distance between the apices of the posterior teeth and the metatarsal shaft varied from 0.68 ± 0.39mm on the distobuccal root (DBR) to 3.93 ± 1.26mm on the palatal root (PR) of the left first molar. In both the male and female groups, a comparable outcome was seen in the maxillary second molar DBR (0.69 ± 1.17mm) from the study. Vertical relations of type 2 and type 2H were the most common types of horizontal relations |
The results of this study indicate that the roots of maxillary molars are closer to the maxillary sinus foundation (MSF) than those of premolars. Additionally, the type 2 vertical and type 2H horizontal distributions of these teeth indicate that CBCT evaluation of the maxillary sinus floor and tooth anatomy should precede treatment planning.” |
|
Chaves LLV et al (2022)[67] |
Brazilian population |
Evaluation of the possibility of maxillary sinus abnormalities using cone-beam computed tomography (CBCT) images in patients who underwent upper jaw dental implants. |
Adult/ Diseased |
A higher risk of mucosal thickening and non-specific opacification was associated with implants placed within 2mm of the cortex of the sinus floor. 13 implants (46.7% of the total) had at least one abnormality related to the sinuses and of the 5 implants (n = 5) that had two-thirds or more of their total length within the maxillary sinus, all of them had at least one abnormality related to the sinuses |
Dental implants placed close to or within the sinus were significantly associated with sinus abnormalities, including non-specific opacification and mucosal thickening, according to this research. |
|
Yeung AWK et al.(2022)[68] |
Chinese population |
Providing a narrative overview of the use of cone beam computed tomography (CBCT) in assessing maxillary sinus anatomy and prevalent diseases |
Adult / Diseased |
Details on the location, morphometric features and detection/visualization rate were provided. Sinus pneumatization, hypoplasia, septa, main and auxiliary sinus ostia and the posterior superior alveolar artery were among the sinus anatomical characteristics that were examined. Membrane thickening in periapical/periodontal lesions, mucous retention cyst and antrolith were all part of the pathology evaluation. |
Procedures that include the extraction of teeth, the insertion of implants, or the elevation of the sinus floor are all performed in close proximity to the sinus floor, thus it is crucial to observe and evaluate the maxillary sinus before these operations |
|
Eid EA et al.(2022)[69] |
Egyptian population |
To accomplish two things: (1) find out whether cone-beam computed tomography images are more accurate than digital periapical radiographs when it comes to evaluating the relationship between the maxillary molar roots and the maxillary sinus floor and (2) identify any periapical radiographic features that might show that the roots are actually sticking out of the sinus cavity. |
Adult/ Diseased |
Periapical radiography showed a 73% accuracy rate in showing the sinus-root link, even if the findings of the two methods were significantly different. In addition, the fact that the dura mater remains intact provides strong evidence (with a reliability of over 70%) that the root is situated outside the sinus and the converse is also true |
In cases when the root is situated outside of the sinus, the digital periapical approach proved to be an appropriate means of evaluating the sinus-root connection. The disruption of the dura mater is a very suggestive periapical sign of root penetration into the maxillary sinus.” |
|
Talwade P et al.(2023)[70] |
Indian population |
They performed research to determine the frequency of accidental paranasal sinus diseases seen on CT scans taken by youngsters |
Pediatric/ Diseased |
The number of participants with incidental sinus diseases was 72 (31.03%) out of a total of 232. Of the patients examined, 36 had several sinus diseases, 28 had involvement of a single sinus and four did not exhibit any growth of the frontal sinus by the age of eleven. At the age range of 6-7 years, four of the participants had disease in numerous sinuses and none of them had developed a frontal sinus |
Almost the same frequency as in adults occurs in the asymptomatic pediatric population when it comes to sinus diseases. Supposedly the children are at risk for upper respiratory tract infections and related complications. In that case, it is important to diagnose them early on to help with orofacial discomfort that has no clear cause. |
|
Kim JH et al.(2023)[71] |
Korean population |
To see if there were any changes in patients who had thickened mucosal tissue in their maxillary sinuses before surgery and whether this was a risk factor for sinusitis after maxillary dental implant |
Adult/ Diseased |
At the post-treatment assessment, the research did not find a significant improvement in maxillary sinus mucosal thickness (MSMT), even when several subgroups were included. |
Better results for patients with preoperative maxillary sinus mucosal thickness may be achieved by cooperation between otolaryngologists and dentists, as well as through radiographic evaluations of the sinuses before surgery. |
|
Fischborn AR et al.(2023)[72] |
Brazilian population |
To evaluate the effectiveness of panoramic radiography (PR) and cone beam computed tomography (CBCT) in identifying infected maxillary sinuses.” |
Adult/ Diseased |
While Panoramic Radiography is currently confined to initial diagnosis, it was determined that CT/CBCT are the most suitable imaging techniques for evaluating pathological alterations in the maxillary sinuses. |
CBCT are the most suitable imaging techniques for evaluating pathological alterations in the maxillary sinuses |
|
Altayar BA et al (2023)[73] |
Chinese population |
To examine CBCT scans to learn more about the maxillary sinus septa's three-dimensional anatomy. |
Adult/ Healthy |
About 47% of sinuses and 63.9% of patients had maxillary sinus septa. Septa were 5.2 mm tall on average. “A total of 30.2% of patients had septa in both maxillae, whereas 15.7% had septa in the right and 18% in the left. There are a lot of septa that started on the floor (54.5%), some in the center (43%), some oriented coronally (66%) and others with a whole arrangement (58.2%). |
Results indicate that the septa prevalence, locations, orientations and morphology are comparable to the greatest levels reported in the literature thus far. Consequently, CBCT imaging of the maxillary sinus is advised for safe dental implantation when sinus floor elevation is being considered.” |
Hypoplasia
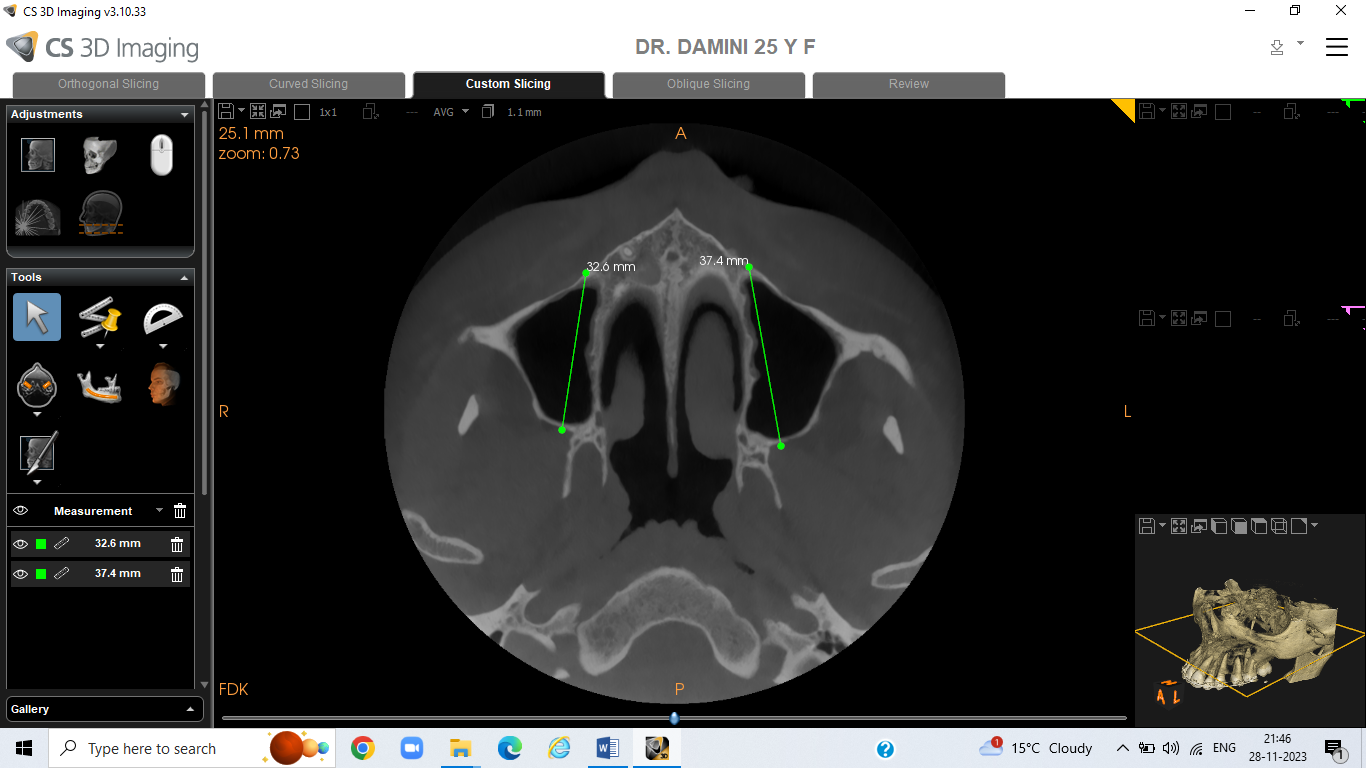
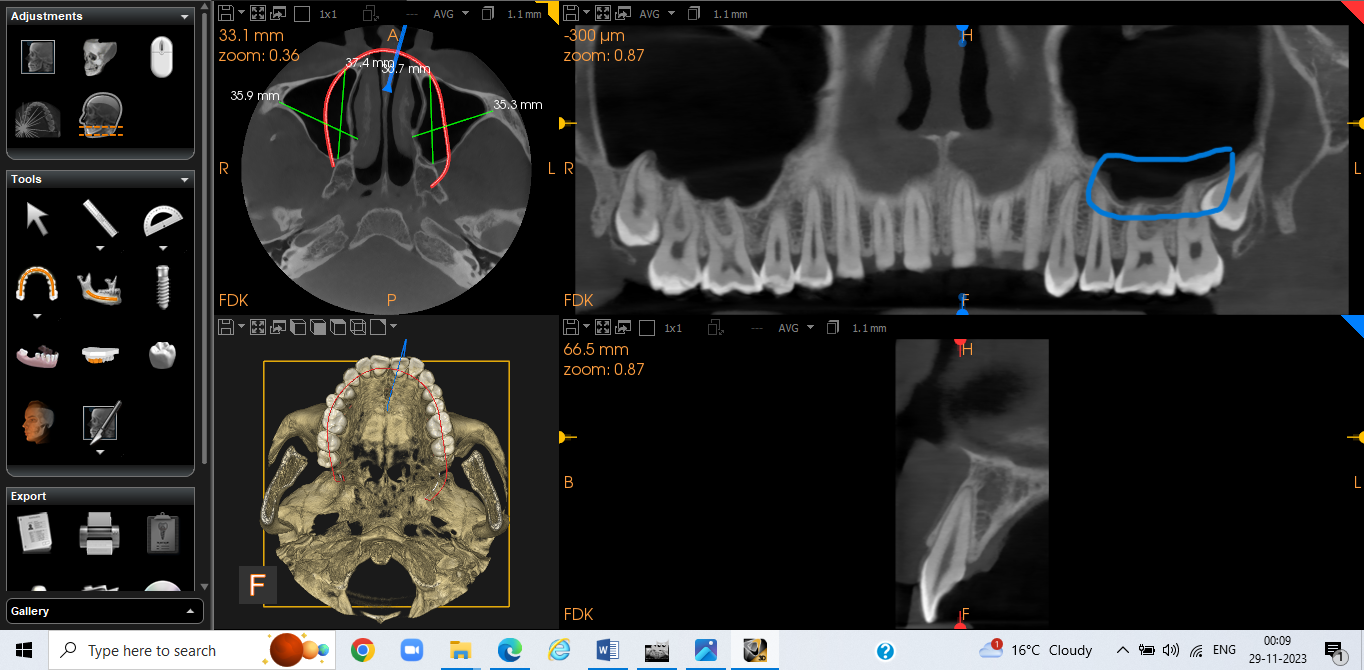
Maxillary sinus hypoplasia (MSH) results in a smaller antrum cavity space than sinus pneumatization. This appears to be a favorable situation at first since there is enough space between the sinus floor and the dentoalveolar area. On the other hand, the frequency of sinus mucosal thickness and obstructed ostium was observed to be significantly higher when there is evidence of MSH in CBCT pictures. According to reports, the frequency of MSH ranges from 0.2% to 50%. [32], [33], [34], [35], [75], [36], [37], [38], [39], [40], [41], [42] The majority of patients fell into either type II (26%) having features like poorly defined or missing infundibular tract, hypoplastic uncinate process and moderate MSH or type I (69% having features of patent infundibular tract, normal uncinate process and mild hypoplasia). A minority (5%) with significant sinus hypoplasia and no uncinate process, was explained by type III. In rare cases, aplasia may be discovered accidentally during CBCT imaging. ([Figure 1]) Sinus hypoplasia did not appear to have an impact on the health or functionality of dentoalveolar frameworks, including open bite, facial asymmetry, or swaying of occlusal plane, aside from sinus healthiness. Any substantial mediation at the back of the mouth needs to be done by a professional who has studied the anatomy and physiology of the maxillary sinuses extensively.[43], [44], [45], [46], [47], [76] There are two possible times when maxillary sinus hypoplasia (MSH) occurs: during embryological development or as a result of injury, iatrogenic factors, or other underlying conditions. Because the hypoplastic sinus lacks a distinctive ostium, it experiences mucosal thickening due to restricted infundibular entrance. On top of that, MSH makes procedures more difficult by causing the horizontal nasal wall to enlarge at its proximal end.[48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60]
Sinus augmentation
A maxillary sinus elevation treatment should be used to enhance the quantity of bone below floor of maxillary antrum in implant situations when the extensively resorbed alveolar bone crest was inadequate to support an implant. Following five to six months of recovery, the volume of the bone graft dropped by 25% on an average, according to recent CBCT studies. There was a mean reduction in graft volume of twenty-eight to forty percent from six months to three years following grafting.[40], [41], [42], [76], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63] But four to seven months following surgery, no such appreciable decrease in the volume of graft was discovered in one CBCT investigation. For an implantation to be effective, the density of bone minerals is just as crucial as volume of bone. It was discovered that there was a strong association between the gray level evaluated at the insertion sites of dental implants in CBCT images and the actual calcified material content calculated at the implant locations. Furthermore, during four to seven months of subsequent follow-up, the gray level of the regions grated by bovine bone fragments stayed steady.[52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63]
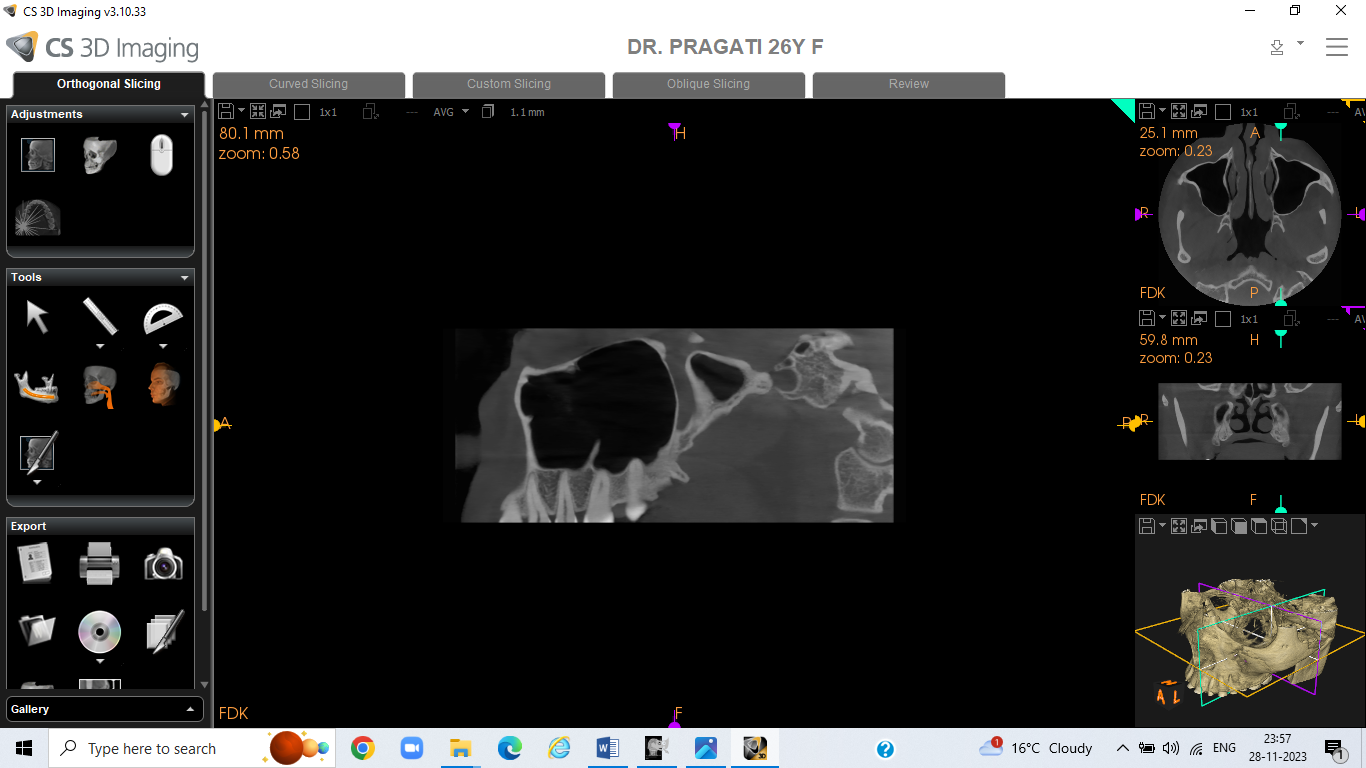
Septa
The maxillary sinus floor is divided into many compartments, called breaks, by the second rate or parallel sinus walls, from which the shape emerges as a converted gothic curve. ([Figure 4]) Anatomist Arthur S. Underwood was the first to study these septa and describe their characteristics; as a result, they are often referred to as Underwood's septa.[7], [8]
Neugebauer J et al.,[31] performed research to evaluate the need for suitable imaging before sinus floor elevation by retrospectively determining the prevalence of septa in the maxillary sinus using computed tomography (CBCT). With respect to the sinuses, 47% of patients and 33.2% of septa were detected. Regarding age, sex and side, there was no statistically significant variation in prevalence. Although 13.7% of individuals with septa had one in each sinus, 24.6% had one in only one sinus. A small percentage of individuals (8.7%) had additional combinations, with up to three septa per sinus. With 256 septa, the first molar area was the most prevalent location for septa.
Li J et al.,[76] “analyzed the maxillary sinus septum of Han nationality in the Jiangsu region using cone-beam computed tomography (CBCT) in conjunction with Simplant software to determine the anatomical basis for oral implant surgery following maxillary sinus lifting and to provide surgical instructions for the procedure. The proportion of the occurrence of maxillary sinus septa in 424 subjects was 44.81% and 21.23% of the subjects (n=90) had multiple sinus septa, while 20.52% had bilateral sinus septa (n=87) in total, 848 maxillary sinuses were included for this analysis and 32.67 percent, or 277 sinuses, had septa. Gender, age and tooth presence/absence had no statistically significant correlation with septa prevalence. The median position of septa in the maxillary sinus was the most common, at 59.94%. In the right maxillary sinus, the average height of the sinus septa was 5.90±3.65mm, whereas in the left sinus, it was 5.54±2.87mm. Sinus septa in the right maxillary sinus averaged 8.15±2.40mm in length, whereas those in the left maxillary sinus averaged 7.88±2.73mm.
Orhan K et al.,[43] used cone beam computed tomography (CBCT) for maxillary sinus surgical procedures to assess the frequency, height, placement and shape of maxillary sinus septa in children with mixed dentition, adults with partial or full dentition and edentulous individuals. Septa involving the maxillary sinus segments were seen in 58% of cases. Septa ranging from totally edentulous (CE) in 13 cases (3.2% of the total), edentate in 198 cases (53.9%) and mixed dentition in 14 cases (3.8%) were seen in the maxillary segments. In terms of septum height, there were no discernible changes according to age or gender. Having said that, compared to edentate and CE individuals, partly edentulous patients had greater maxillary sinus septa. Extensive examination using a suitable radiographic approach was important to minimize any difficulties during sinus surgery, since septa of varying heights and courses occurred in all areas of the maxillary sinus.
Pathology
Membrane thickening associated with periapical lesions
Thickening of the sinus membrane was frequently observed in teeth with endodontic involvement. Numerous studies have reported on it. In a single research study, the membrane of the sinuses was shown to be much thicker in individuals with concomitant teeth exhibiting apical disease than normal controls.[22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32] According to an additional research study, the average incidence of membrane thickening was found to be 41.5% in patients with apical periodontitis who had no associated teeth. However, this number rose to approximately 70% in patients who had visible minor modifications in the structure of the bone to an established radiolucent periapical region and it reached 100% in individuals with severe cases of the disease.[33], [34], [35], [75], [36]
A more contemporary study's outcomes supported earlier findings, showing that teeth having periapical lesions were more probable to be related to sinuses with greater than two mm membrane thickening. When periapical lesions are present, the likelihood of membrane thickening might increase up to three times higher than in the absence of periapical lesions. For sinus membrane thickening to occur, the periapical lesion did not always need to come into contact with or penetrate the sinus floor. The degree of thickening was likewise unaffected by the quantity of related root canal treatments.[37], [38], [39], [40], [41], [42], [76], [43]
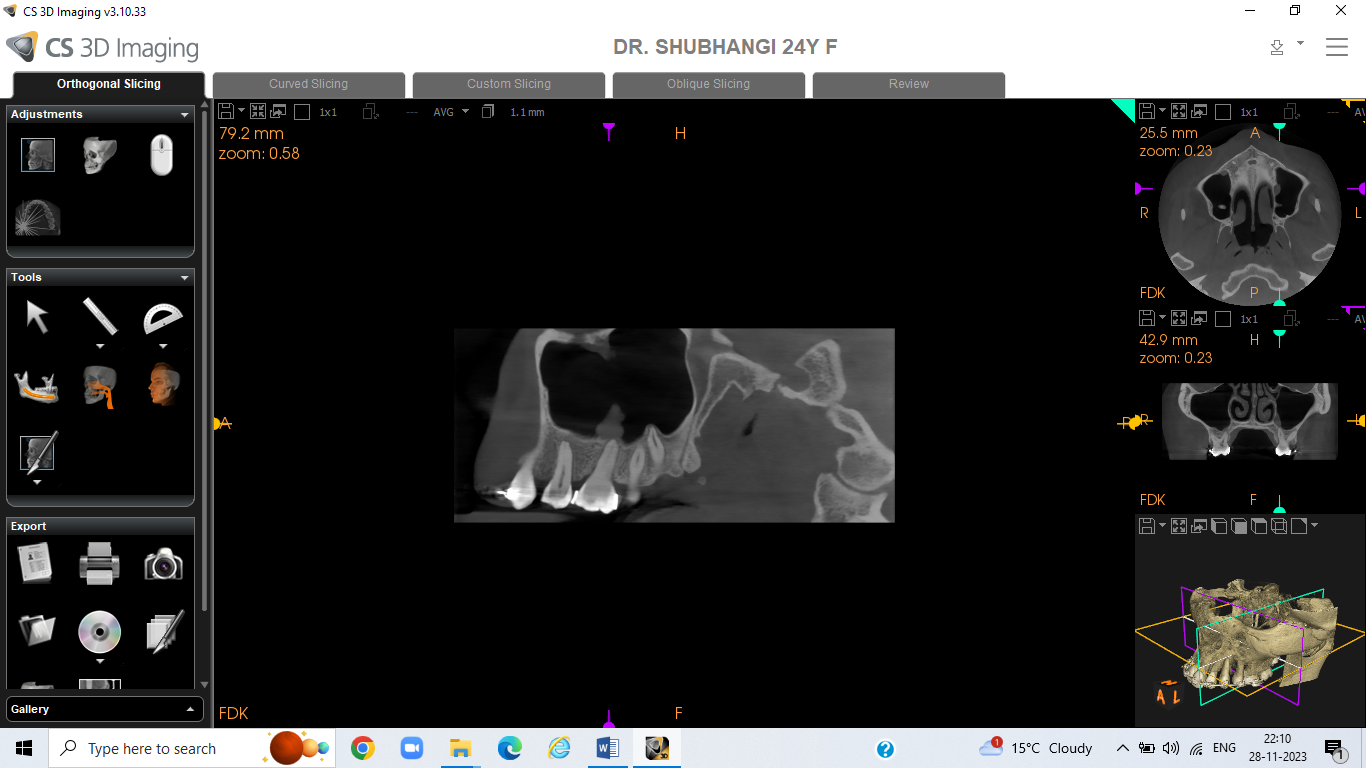
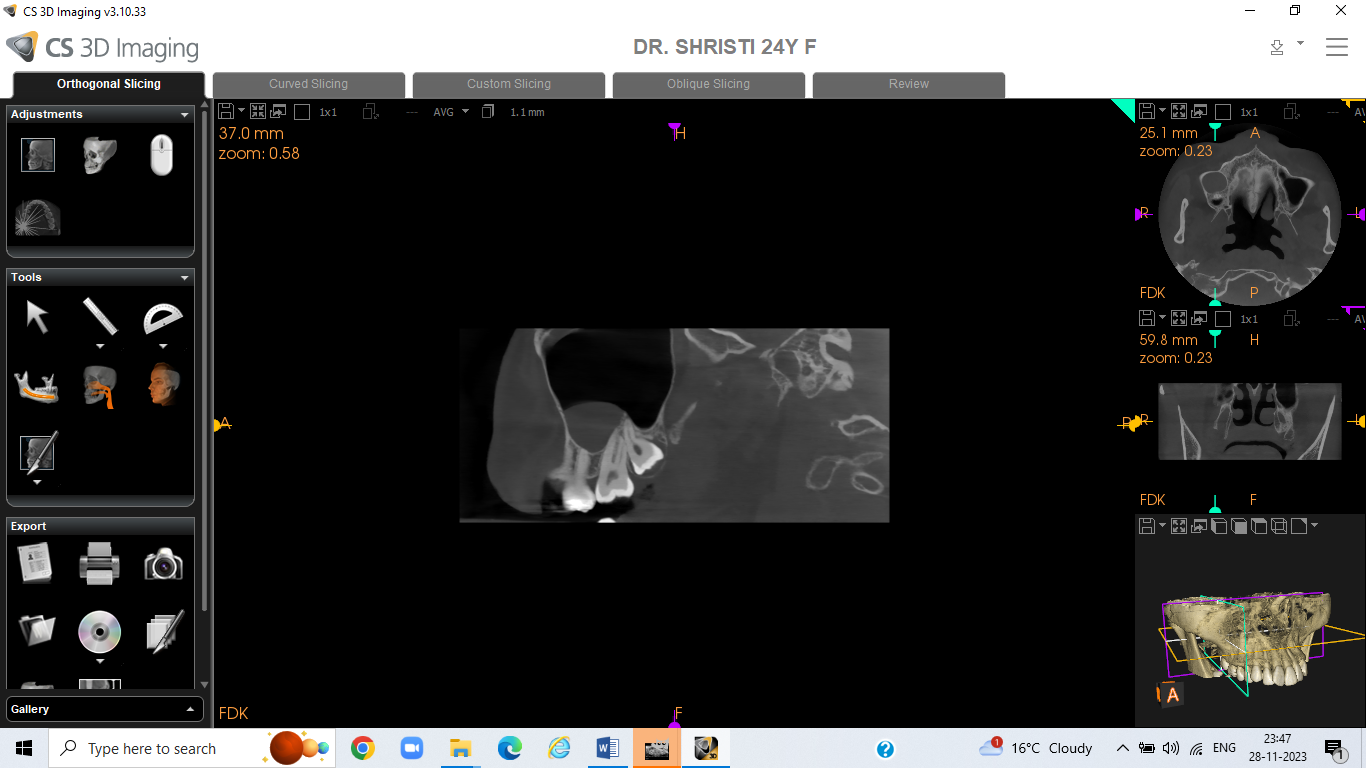
Membrane thickening associated with periodontal lesions
Membrane thickening appeared to be more common in teeth with more extensive periodontal degeneration, which is similar to periapical lesions. Those with extensive periodontal bone loss had a 4.6-fold higher likelihood of membrane thickening compared to those with minor bone loss. ([Figure 5]) Membrane thickening was 1.6 and 3.5 times greater more common in individuals experiencing class II and class III furcation lesions, respectively, compared to those lacking furcation involvement. Additionally, thickening of maxillary sinus membrane was found to be 2.4–5.6 fold more common when there were any transverse intra-bony pockets than in the absence of such pockets. At four months, the thickening of sinus membrane would completely resolve with the removal of the periodontally affected tooth.[40], [41], [42], [76], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55]
Mucous retention cyst (MRC)
A common location for MRCs is the maxillary sinus; ten percent to thirty percent of the maxillary sinus had MRCs. Within a single sinus, up to four MRCs have been recorded. Rather than on the roof, MRCs were more frequently found at the walls of maxillary antrum and floor. If a tooth had endodontic therapy, periapical lesions, or had significant bone loss, the likelihood of MRCs on the floor of maxillary antrum was increased.[34], [35], [75], [36], [37], [38], [39], [40], [41], [42], [76], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54]
Antrolith
A calcified lump in the maxillary antrum is called an antrolith. Between 0.6% and 8.4% of maxillary antrum had antroliths. They could be amorphous, linear, or punctate. Instead of being in the premolar area, the majority of them were situated on the floor of sinus in the molar area. The highest cross-sectional area estimated based on coronal slices revealed that the measurement of an antrolith ranged from 1 to 91mm2. According to another study, the average measurements were 3.5± 2.1mm in height, 4.1± 2.9mm in breadth and 5.6± 4.4mm in length.[31], [32], [33], [34], [35], [75], [36], [37], [38], [39], [40], [41], [42], [76], [43], [44], [45], [46], [47], [48], [49], [50], [51] Although it would seem intuitively that having antroliths would increase the likelihood of membrane perforation after implant placement when sinus floor elevation is occurring at the same time, however study findings did not support this theory.[21], [22], [23], [24], [25], [26], [27], [28], [29]
Foreign bodies
Latrogenic entry of foreign bodies into the maxillary sinus can occasionally happen because the dentoalveolar area and the maxillary sinus floor are so close together. CBCT imaging can be used to pinpoint the foreign substances. For instance, one study found that 27 individuals had dental implants, tooth pieces, whole teeth, dental burs, root filling material, dental impression material placed inside their maxillary sinus.[61], [62], [63], [64], [65] During root canal therapy, a perforated root could allow a large amount of root filling material to be forced into the maxillary antrum cavity. In the meantime, even in cases where a substantially atrophic edentulous ridge was present, the majority of dental implant patients that were placed into the sinus did not have a preoperative CBCT exam.[42], [76], [43], [44], [45], [46], [47], [48], [49]
Conclusion
A number of variables, including the maxillary sinus's complicated anatomy, increase the risk of surgical difficulties around sinus floor elevation. Prior to surgery, a CBCT three-dimensional radiographic examination might aid in diagnosis and treatment planning. Analytical features with varying frequencies have been documented in earlier research. In addition, other studies found different correlations between different bones and factors including age, gender and oral health. “While chest computed tomography (CBCT) does expose patients to slightly more radiation than regular panoramic radiography for dento maxillofacial imaging, it is still a viable option for low-cost dose-paring scans compared to conventional medical computed tomography (MDCT).
Also, CBCT has less beam hardening artifacts from dental materials (such as amalgam, crowns and implants) compared to MSCT. Comprehending the various anatomical and pathologic features in the sinuses is essential for minimizing the risk of postoperative problems after maxillary sinus floor lifts and other procedures in this area.” Recognizing anatomic variations of the maxillary sinuses in CBCT is noteworthy, considering the importance of the maxillary sinuses as clinically relevant anatomic structures and the need for precise and conclusive radiological assessment.
Anatomical differences of the maxillary sinus are often seen in maxillary CBCT, OPG and PNS. Due to the fact that these diseases might impact surgical planning and need specialist treatments, it is essential for them to be identified in dental practice. Without a doubt, CBCT preoperative imaging is useful for evaluating the normal variations and maxillary sinus morphology, which may be utilized to modify the surgical treatment plan for effective and satisfactory outcomes.
Source of Funding
None.
Conflict of Interest
None.
References
- M Faramarzie, AR Babaloo, SG Oskouei. Prevalence, height, and location of antral septa in Iranian patients undergoing maxillary sinus lift. J Periodontol Implant Dent 2009. [Google Scholar]
- H Stammberger. Endoscopic endonasal surgery--concepts in treatment of recurring rhinosinusitis. Part I. Anatomic and pathophysiologic considerations. Otolaryngol Head Neck Surg 1986. [Google Scholar]
- DT Weed, RR Cole. Maxillary sinus hypoplasia and vertical dystopia of the orbit. Laryngoscope 1994. [Google Scholar]
- PKD Kapoor, BN Kumar, SD Watson. Maxillary sinus hypoplasia. J Laryngol Otol 2002. [Google Scholar]
- B Pommer, C Ulm, M Lorenzoni, R Palmer, G Watzek, W Zechner. Prevalence, location and morphology of maxillary sinus septa: systematic review and meta analysis. J Clin Periodontol 2012. [Google Scholar]
- MJ Kim, UW Jung, CS Kim, KD Kim, SH Choi, CK Kim. Maxillary sinus septa: prevalence, height, location, and morphology. A reformatted computed tomography scan analysis. J Periodontol 2006. [Google Scholar]
- R Koymen, N Gocmen-Mas, U Karacayli, K Ortakoglu, T Ozen, AC Yazici. Anatomic evaluation of maxillary sinus septa: surgery and radiology. Clin Anat 2009. [Google Scholar]
- G Krennmair, C Ulm, H Lugmayr. Maxillary sinus septa: incidence, morphology and clinical implications. J Craniomaxillofac Surg 1997. [Google Scholar]
- G Krennmair, CW Ulm, H Lugmayr, P Solar. The incidence, location, and height of maxillary sinus septa in the edentulous and dentate maxilla. J Oral Maxillofac Surg 1999. [Google Scholar]
- M Naitoh, Y Suenaga, S Kondo, K Gotoh, E Ariji. Assessment of maxillary sinus septa using cone-beam computed tomography: etiological consideration. Clin Implant Dent Relat Res 2009. [Google Scholar]
- A Mavrodi, G Paraskevas. Evolution of the paranasal sinuses' anatomy through the ages. Anat Cell Biol 2013. [Google Scholar]
- AN Castruita, NL Serna, SG López. Prenatal development of the maxillary sinus: a perspective for paranasal sinus surgery. Otolaryngol Head Neck Surg 2012. [Google Scholar]
- S Standring. . Gray's anatomy: the anatomical basis of clinical practice 2015. [Google Scholar]
- J Lang. . Clinical anatomy of the nose, nasal cavity, and paranasal sinuses 1989. [Google Scholar]
- JA Duncavage, SS Becker. . The maxillary sinus: medical and surgical management 2011. [Google Scholar]
- M Chanavaz. Maxillary sinus: anatomy, physiology, surgery, and bone grafting related to implantology: eleven years of surgical experience (1979-1990). J Oral Implantol 1990. [Google Scholar]
- JA Eberhardt, M Torabinejad, EL Christiansen. A computed tomographic study of the distances between the maxillary sinus floor and the apices of the maxillary posterior teeth. Oral Surg Oral Med Oral Pathol 1992. [Google Scholar]
- C Kilic, K Kamburoglu, SP Yuksel, T Ozen. An assessment of the relationship between the maxillary sinus floor and the maxillary posterior teeth root tips using dental cone-beam computerized tomography. Eur J Dent 2010. [Google Scholar]
- GD Roque-Torres, LR Ramirez-Sotelo, SL Vaz, SM Bóscolo, FN Bóscolo. Association between maxillary sinus pathologies and healthy teeth. Braz J Otorhinolaryngol 2016. [Google Scholar]
- MJ Kim, UW Jung, CS Kim, KD Kim, SH Choi, CK Kim. Maxillary sinus septa: prevalence, height, location, and morphology: a reformatted computed tomography scan analysis. J Periodontol 2006. [Google Scholar]
- G Krennmair, CW Ulm, H Lugmayr, P Solar. The incidence, location, and height of maxillary sinus septa in the edentulous and dentate maxilla. J Oral Maxillofac Surg 1999. [Google Scholar]
- AS Underwood. An inquiry into the anatomy and pathology of the maxillary sinus. J Anat Physiol 1910. [Google Scholar]
- WJ Lee, SJ Lee, HS Kim. Analysis of location and prevalence of maxillary sinus septa. J Periodontal Implant Sci 2010. [Google Scholar]
- LM Ferrín, CC García, SG Gil, MP Diago, MP Diago. Prevalence, location, and size of maxillary sinus septa: panoramic radiograph versus computed tomography scan. J Oral Maxillofac Surg 2011. [Google Scholar]
- DV Plata, LR Hovey, CC Peach, ME Alder. Maxillary sinus septa: a 3-dimensional computerized tomographic scan analysis. Int J Oral Maxillofac Implants 2002. [Google Scholar]
- HG Santana, MP Diago, JG Carbó, MS Bröker. A study of the septa in the maxillary sinuses and the subantral alveolar processes in 30 patients. J Oral Implantol 2007. [Google Scholar]
- GW Bell, BB Joshi, RI Macleod. Maxillary sinus disease: diagnosis and treatment. Br Dent J 2011. [Google Scholar]
- L Kqiku, R Biblekaj, AH Weiglein, X Kqiku, P Städtler. Arterial blood architecture of the maxillary sinus in dentate specimens. Croat Med J 2013. [Google Scholar]
- D Flanagan. Arterial supply of maxillary sinus and potential for bleeding complication during lateral approach sinus elevation. Implant Dent 2005. [Google Scholar]
- K Lovasova, D Kachlik, M Rozpravkova, M Matusevska, J Ferkova, D Kluchova. Three-dimensional CAD/CAM imaging of the maxillary sinus in ageing process. Ann Anat 2018. [Google Scholar]
- J Neugebauer, L Ritter, RA Mischkowski, T Dreiseidler, P Scherer, M Ketterle. Evaluation of maxillary sinus anatomy by cone-beam CT prior to sinus floor elevation. Int J Oral Maxillofac Implants 2010. [Google Scholar]
- BA Hassan. Reliability of periapical radiographs and orthopantomograms in detection of tooth root protrusion in the maxillary sinus: correlation results with cone beam computed tomography. J Oral Maxillofac Res 2010. [Google Scholar]
- P Pazera, MM Bornstein, A Pazera, P Sendi, C Katsaros. Incidental maxillary sinus findings in orthodontic patients: a radiographic analysis using cone-beam computed tomography (CBCT). Orthod Craniofac Res 2011. [Google Scholar]
- L Ritter, J Lutz, J Neugebauer, M Scheer, T Dreiseidler, MJ Zinser. Prevalence of pathologic findings in the maxillary sinus in cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011. [Google Scholar]
- JP Lana, PM Carneiro, VDC Machado, PE De Souza, FR Manzi, MCR Horta. Anatomic variations and lesions of the maxillary sinus detected in cone beam computed tomography for dental implants. Clin Oral Implants Res 2012. [Google Scholar]
- IC Rege, TO Sousa, CR Leles, EF Mendonça. Occurrence of maxillary sinus abnormalities detected by cone beam CT in asymptomatic patients. BMC Oral Health 2012. [Google Scholar]
- A Gracco, SI parenti, C Ioele, GA Bonetti, E Stellini. Prevalence of incidental maxillary sinus findings in Italian orthodontic patients: a retrospective cone-beam computed tomography study. Korean J Orthod 2012. [Google Scholar]
- DD Brüllmann, I Schmidtmann, S Hornstein, RK Schulze. Correlation of cone beam computed tomography (CBCT) findings in the maxillary sinus with dental diagnoses: a retrospective cross-sectional study. Clin Oral Investig 2012. [Google Scholar]
- Y Lu, Z Liu, L Zhang, X Zhou, Q Zheng, X Duan. Associations between maxillary sinus mucosal thickening and apical periodontitis using cone-beam computed tomography scanning: a retrospective study. J Endod 2012. [Google Scholar]
- L Tolstunov, D Thai, L Arellano. Implant-guided volumetric analysis of edentulous maxillary bone with cone-beam computerized tomography scan. Maxillary sinus pneumatization classification. J Oral Implantol 2012. [Google Scholar]
- I Dobele, L Kise, P Apse, G Kragis, A Bigestans. Radiographic assessment of findings in the maxillary sinus using cone-beam computed tomography. Stomatologija 2013. [Google Scholar]
- M Nazri, SI Bux, TF Tengku-Kamalden, KH Ng, Z Sun. Incidental detection of sinus mucosal abnormalities on CT and MRI imaging of the head. Quant Imaging Med Surg 2013. [Google Scholar]
- K Orhan, BK Seker, S Aksoy, H Bayindir, A Berberoğlu, E Seker. Cone beam CT evaluation of maxillary sinus septa prevalence, height, location and morphology in children and an adult population. Med Princ Pract 2013. [Google Scholar]
- M Shahbazian, C Vandewoude, J Wyatt, R Jacobs. Comparative assessment of panoramic radiography and CBCT imaging for radiodiagnostics in the posterior maxilla. Clin Oral Investig 2014. [Google Scholar]
- K Shiki, T Tanaka, S Kito, NW Sato, SM Takeda, M Oda. The significance of cone beam computed tomography for the visualization of anatomical variations and lesions in the maxillary sinus for patients hoping to have dental implant-supported maxillary restorations in a private dental office in Japan. Head Face Med 2014. [Google Scholar]
- T Vogiatzi, D Kloukos, WC Scarfe, MM Bornstein. Incidence of anatomical variations and disease of the maxillary sinuses as identified by cone beam computed tomography: a systematic review. Int J Oral Maxillofac Implants 2014. [Google Scholar]
- MS Block, K Dastoury. Prevalence of sinus membrane thickening and association with unhealthy teeth: a retrospective review of 831 consecutive patients with 1,662 cone-beam scans. J Oral Maxillofac Surg 2014. [Google Scholar]
- M Raghav, FR Karjodkar, S Sontakke, K Sansare. Prevalence of incidental maxillary sinus pathologies in dental patients on cone-beam computed tomographic images. Contemp Clin Dent 2014. [Google Scholar]
- S Shahidi, B Zamiri, SM Danaei, S Salehi, S Hamedani. Evaluation of Anatomic Variations in Maxillary Sinus with the Aid of Cone Beam Computed Tomography (CBCT) in a Population in South of Iran. J Dent (Shiraz) 2016. [Google Scholar]
- XM Tian, L Qian, XZ Xin, B Wei, Y Gong. An Analysis of the Proximity of Maxillary Posterior Teeth to the Maxillary Sinus Using Cone-beam Computed Tomography. J Endod 2016. [Google Scholar]
- MM Bornstein, C Seiffert, LM Ferrín, I Fodich, R Jacobs, D Buser. An Analysis of Frequency, Morphology, and Locations of Maxillary Sinus Septa Using Cone Beam Computed Tomography. Int J Oral Maxillofac Implants 2016. [Google Scholar]
- MT Alkurt, I Peker, S Degerli, AR Cebeci, E Sadik. Comparison of cone-beam computed tomography and panoramic radiographs in detecting maxillary sinus septa. J Istanb Univ Fac Dent 2016. [Google Scholar]
- JA Ali, JVD Vilalta, M Melo, L Bagán, MC Soldini, CD Nardo. What is the frequency of anatomical variations and pathological findings in maxillary sinuses among patients subjected to maxillofacial cone beam computed tomography? A systematic review.. Med Oral Patol Oral Cir Bucal 2017. [Google Scholar]
- M Schriber, TV Arx, P Sendi, R Jacobs, VG Suter, MM Bornstein. Evaluating Maxillary Sinus Septa Using Cone Beam Computed Tomography: Is There a Difference in Frequency and Type Between the Dentate and Edentulous Posterior Maxilla?. Int J Oral Maxillofac Implants 2017. [Google Scholar]
- F Taleghani, M Tehranchi, S Shahab, Z Zohri. Prevalence, Location, and Size of Maxillary Sinus Septa: Computed Tomography Scan Analysis. J Contemp Dent Pract 2017. [Google Scholar]
- W Sun, K Xia, L Tang, C Liu, L Zou, J Liu. Accuracy of panoramic radiography in diagnosing maxillary sinus-root relationship: A systematic review and meta-analysis. Angle Orthod 2018. [Google Scholar]
- A Hungerbühler, C Rostetter, HT Lübbers, M Rücker, B Stadlinger. Anatomical characteristics of maxillary sinus septa visualized by cone beam computed tomography. Int J Oral Maxillofac Surg 2019. [Google Scholar]
- S Constantine, B Clark, A Kiermeier, PP Anderson. Panoramic radiography is of limited value in the evaluation of maxillary sinus disease. Oral Surg Oral Med Oral Pathol Oral Radiol 2019. [Google Scholar]
- A Terlemez, M Tassoker, M Kizilcakaya, M Gulec. Comparison of cone-beam computed tomography and panoramic radiography in the evaluation of maxillary sinus pathology related to maxillary posterior teeth: Do apical lesions increase the risk of maxillary sinus pathology. Imaging Sci Dent 2019. [Google Scholar]
- K Kirkham-Ali, La M Sher, J Sholapurkar, A. Comparison of cone-beam computed tomography and panoramic imaging in assessing the relationship between posterior maxillary tooth roots and the maxillary sinus: A systematic review. J Investig Clin Dent 2019. [Google Scholar]
- S Themkumkwun, J Kitisubkanchana, A Waikakul, K Boonsiriseth. Maxillary molar root protrusion into the maxillary sinus: a comparison of cone beam computed tomography and panoramic findings. Int J Oral Maxillofac Surg 2019. [Google Scholar]
- AC Lang, RK Schulze. Detection accuracy of maxillary sinus floor septa in panoramic radiographs using CBCT as gold standard: a multi-observer receiver operating characteristic (ROC) study. Clin Oral Investig 2019. [Google Scholar]
- M S Al-Zahrani, Al-Ahmari Mm Al-Zahrani, A A Al-Mutairi, K D Zawawi, K H. Prevalence and morphological variations of maxillary sinus septa in different age groups: a CBCT analysis. Ann Saudi Med 2020. [Google Scholar]
- J Pei, J Liu, Y Chen, Y Liu, X Liao, J Pan. Relationship between maxillary posterior molar roots and the maxillary sinus floor: Cone-beam computed tomography analysis of a western Chinese population. J Int Med Res 2020. [Google Scholar]
- ME Toprak, MS Ataç. Maxillary sinus septa and anatomical correlation with the dentition type of sinus region: a cone beam computed tomographic study. Br J Oral Maxillofac Surg 2021. [Google Scholar]
- KS Hameed, E Elaleem, D Alasmari, D. Radiographic evaluation of the anatomical relationship of maxillary sinus floor with maxillary posterior teeth apices in the population of Al-Qassim, Saudi Arabia, using cone beam computed tomography. Saudi Dent J 2021. [Google Scholar]
- LLV Chaves, LPL Rosado, SM Piccolo, LM Ferreira, K Kamburoglu, RB Junqueira. Evaluation of the Maxillary Sinus of Patients with Maxillary Posterior Implants: A CBCT Cross-Sectional Study. Diagnostics (Basel) 2022. [Google Scholar]
- AWK Yeung, KF Hung, DTS Li, YY Leung. The Use of CBCT in Evaluating the Health and Pathology of the Maxillary Sinus. Diagnostics 2022. [Google Scholar]
- EA Eid, FM El-Badawy, WM Hamed. Accuracy of intraoral digital radiography in assessing maxillary Sinus-Root relationship compared to CBCT. Saudi Dent J 2022. [Google Scholar]
- P Talwade, PS Deshpande, S Pene, S Kumar, V Kudagi, M Limaye. Incidental Paranasal Sinus Findings on Computed Tomography Images of Pediatric Patients: A Cross-sectional Prevalence Study. Int J Clin Pediatr Dent 2023. [Google Scholar]
- JH Kim, EJ Min, Y Ko, DH Kim, JB Park. Change in Maxillary Sinus Mucosal Thickness in Patients with Preoperative Maxillary Sinus Mucosal Thickening as Assessed by Otolaryngologists: A Retrospective Study. Medicina (Kaunas) 2023. [Google Scholar]
- AR Fischborn, JD Andreis, LM Wambier, CM Pedroso, M Claudino, GCN Franco. Performance of panoramic radiography compared with computed tomography in the evaluation of pathological changes in the maxillary sinuses: a systematic review and meta-analysis. Dentomaxillofac Radiol 2023. [Google Scholar]
- BA Altayar, B Al-Tayar, W Lin, SN Al-Wesabi, EA Al-Shujaa, K Sakran. Cone-beam computed tomographic analysis of maxillary sinus septa among Yemeni population: a cross-sectional study. BMC Oral Health 2023. [Google Scholar]
- MS Alassaf, A Alolayan, E Almuzaini, AA Masoudi, K Alturki, AK Alsaeedi. Prevalence and Characteristics of the Maxillary Sinus Septa in a Saudi Arabian Sub-population: A Retrospective Cone Beam Computed Tomography (CBCT)-Based Study. Cureus 2023. [Google Scholar]
- B Pommer, C Ulm, M Lorenzoni, R Palmer, G Watzek, W Zechner. Prevalence, location and morphology of maxillary sinus septa: systematic review and meta-analysis. J Clin Periodontol 2012. [Google Scholar]
- J Li, ZX Zhou, ZY Yuan, H Yuan, C Sun, N Chen. An anatomical study of maxillary sinus septum of Han population in Jiangsu region using cone-beam CT. Shanghai Kou Qiang Yi Xue 2013. [Google Scholar]
